Sessions with Suicidal Ideation
When suicidal ideation is mentioned by the client in session, we need to take extra action and precaution with our charting. This will also apply to situations with any type of abuse being reported.
Some practical things to consider
The highest likelihood of chart notes being subpoenaed will occur when there is suicidal ideation or abuse taking place. You should work to cover your bases in ensuring client safety and following ethical guidelines for risk assessment. But this also means that you should be extra-editing your chart notes, getting them reviewed by your supervisor and/or site supervisor AND getting them signed off as soon as possible. The longer it takes for a chart note to be signed, the more reputable it is. Additionally, heaven forbid something were to happen following the session but BEFORE your chart note is signed, in a court of law that may not be good - you could have added anything you wanted to that chart note in that time. So, get the notes signed asap.
What to do in Session
When suicidal ideation shows up in session, you should work to make sure you stay calm and curious and gather further information, validate feelings, thank them for sharing and being vulnerable and work to explore the thoughts/problems. You will also want to discuss with them any limits of confidentiality so they are aware of your limitation as a therapist.
From there, you want to assess the clients level of risk. You may which to explore protective factors and risk factors. You want to explore frequency and severity of thoughts. You should ask some direct questions such as "Do you have a plan?" "do you have means to commit suicide?" "Are you a current harm to yourself or anyone else?" These direct questions mean you will hopefully receive direct answers!
You also want to pay attention to their physical presence and other tangible cues - are they looking away? are they dissociated? do they appear grounded? are they crying?
At the end of session you should be checking in to make sure the client is leaving safely.
Add the risk assessment to the chart note to be sure you cover your bases in session and chart appropriately. Go to the bottom left of the chartt note and hit "add item" then click "risk assessment". Follow the prompts.
Charting
"overchart" - typically, we try to be concise in our charting, however, these situations often warrant us as the therapist "doing more" and require specific information to be reported. So, I always say, over chart in these instances!
Add the risk assessment to the chart note to be sure you cover your bases in session and chart appropriately. Go to the bottom left of the chartt note and hit "add item" then click "risk assessment". Follow the prompts.
the goal here is to accurately report what the client is experiencing, while protecting them, and also illustrate that you did everything you should and are supposed to do to ensure the clients safety before the end of session.
Only include things in the chart note that you've actually done and that are truthful
Under the interventions section you want to include...
that you've covered confidentiality limitations
any direct assessments used
any safety questions asked
as usual, any interventions provided
Under the topics section you want to include...
what the client reported in response to the questions asked
try to keep their reporting of SI or abuse to the point and non detailed to protect the client, unless necessary for treatment to include it.
Under themes/impressions you want to include...
"observations" - list anything you observed that illustrated safety
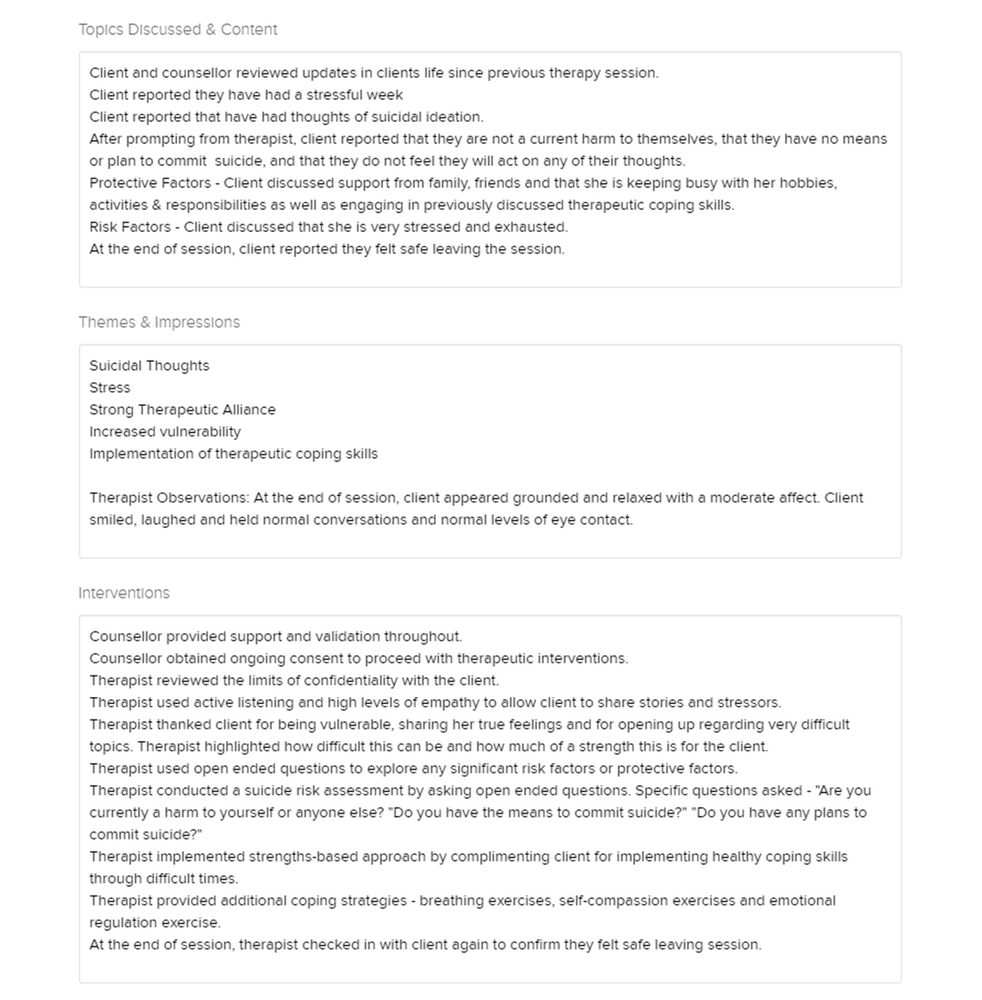
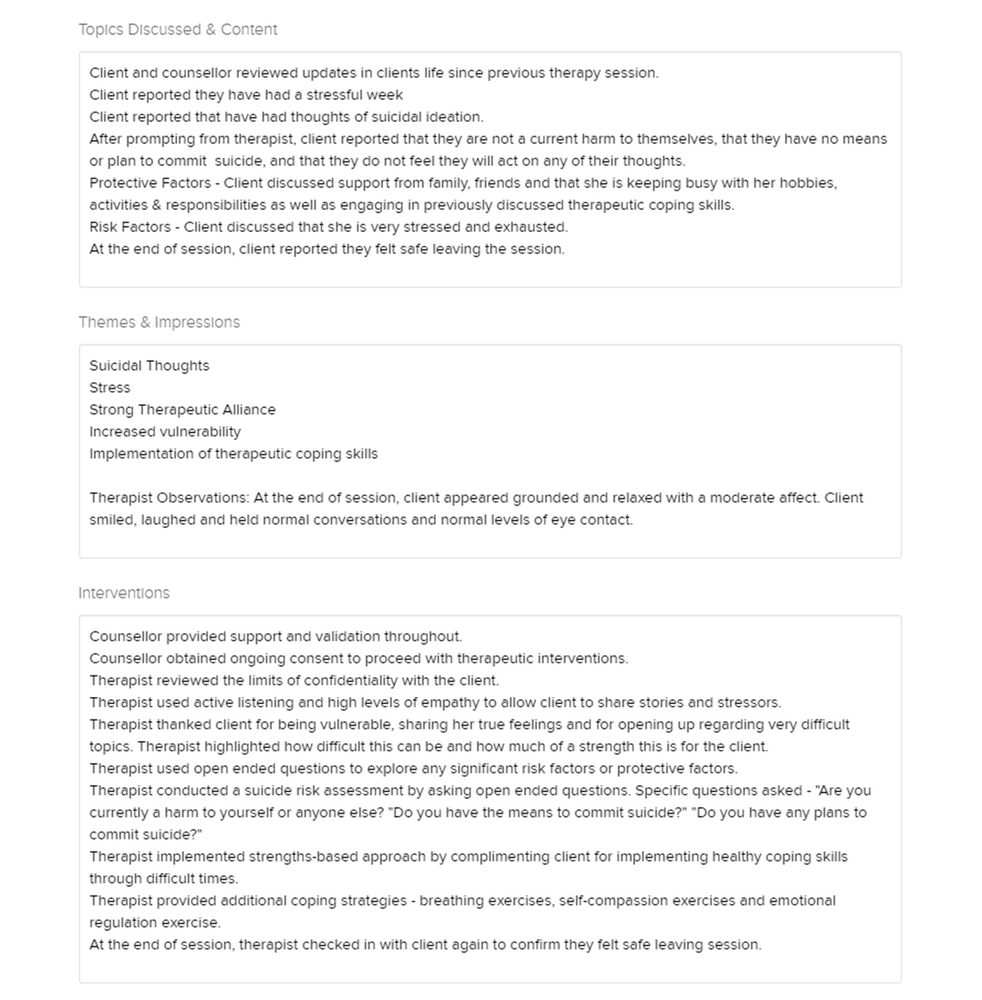
Here's a sample SI chart note!
*PLEASE NOTE* This is a fake chart note and does not belong to a client. This was written exclusively for training purposes.
Safe and Effective Use of Self
Suicidal ideation/risk can be jarring in session and may stir up a variety of emotions in you! Our recommendation is to book a session with your supervisor as soon as possible to be able to debrief clinically, and from a SEUS standpoint. While Brittany cannot provide clinical supervsion, she is available for a debrief and to discuss or vent/process. Also, feel free to turn to your colleagues! It's important that you feel supported and that you have a place to process. Lots of extra self care is highly recommended as these things can shake you up!
Some practical things to consider
The highest likelihood of chart notes being subpoenaed will occur when there is suicidal ideation or abuse taking place. You should work to cover your bases in ensuring client safety and following ethical guidelines for risk assessment. But this also means that you should be extra-editing your chart notes, getting them reviewed by your supervisor and/or site supervisor AND getting them signed off as soon as possible. The longer it takes for a chart note to be signed, the more reputable it is. Additionally, heaven forbid something were to happen following the session but BEFORE your chart note is signed, in a court of law that may not be good - you could have added anything you wanted to that chart note in that time. So, get the notes signed asap.
What to do in Session
When suicidal ideation shows up in session, you should work to make sure you stay calm and curious and gather further information, validate feelings, thank them for sharing and being vulnerable and work to explore the thoughts/problems. You will also want to discuss with them any limits of confidentiality so they are aware of your limitation as a therapist.
From there, you want to assess the clients level of risk. You may which to explore protective factors and risk factors. You want to explore frequency and severity of thoughts. You should ask some direct questions such as "Do you have a plan?" "do you have means to commit suicide?" "Are you a current harm to yourself or anyone else?" These direct questions mean you will hopefully receive direct answers!
You also want to pay attention to their physical presence and other tangible cues - are they looking away? are they dissociated? do they appear grounded? are they crying?
At the end of session you should be checking in to make sure the client is leaving safely.
Add the risk assessment to the chart note to be sure you cover your bases in session and chart appropriately. Go to the bottom left of the chartt note and hit "add item" then click "risk assessment". Follow the prompts.
Charting
"overchart" - typically, we try to be concise in our charting, however, these situations often warrant us as the therapist "doing more" and require specific information to be reported. So, I always say, over chart in these instances!
Add the risk assessment to the chart note to be sure you cover your bases in session and chart appropriately. Go to the bottom left of the chartt note and hit "add item" then click "risk assessment". Follow the prompts.
the goal here is to accurately report what the client is experiencing, while protecting them, and also illustrate that you did everything you should and are supposed to do to ensure the clients safety before the end of session.
Only include things in the chart note that you've actually done and that are truthful
Under the interventions section you want to include...
that you've covered confidentiality limitations
any direct assessments used
any safety questions asked
as usual, any interventions provided
Under the topics section you want to include...
what the client reported in response to the questions asked
try to keep their reporting of SI or abuse to the point and non detailed to protect the client, unless necessary for treatment to include it.
Under themes/impressions you want to include...
"observations" - list anything you observed that illustrated safety
Here's a sample SI chart note!
*PLEASE NOTE* This is a fake chart note and does not belong to a client. This was written exclusively for training purposes.
Safe and Effective Use of Self
Suicidal ideation/risk can be jarring in session and may stir up a variety of emotions in you! Our recommendation is to book a session with your supervisor as soon as possible to be able to debrief clinically, and from a SEUS standpoint. While Brittany cannot provide clinical supervsion, she is available for a debrief and to discuss or vent/process. Also, feel free to turn to your colleagues! It's important that you feel supported and that you have a place to process. Lots of extra self care is highly recommended as these things can shake you up!